
A vial of vaccine with a syringe in the background | Source: Getty Images
Measles Outbreak Worsens in U.S. State as Health Officials Confirm Tragic Fatality Amid Rising Cases
Texas Confirms First Measles-Related Death as Cases Surge in South Plains and Panhandle Regions
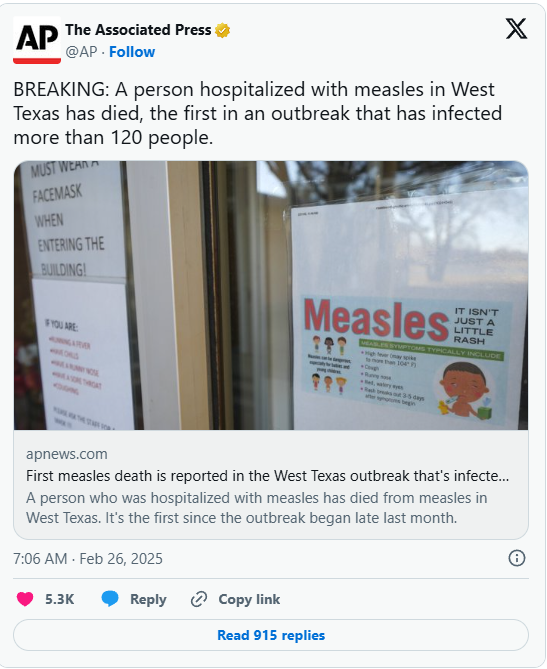
Health officials have reported Texas’ first measles-related fatality amid a growing outbreak. The Texas Department of State Health Services (DSHS) confirmed the tragic death on February 26, 2025, as cases continue to rise in the South Plains and Panhandle regions.
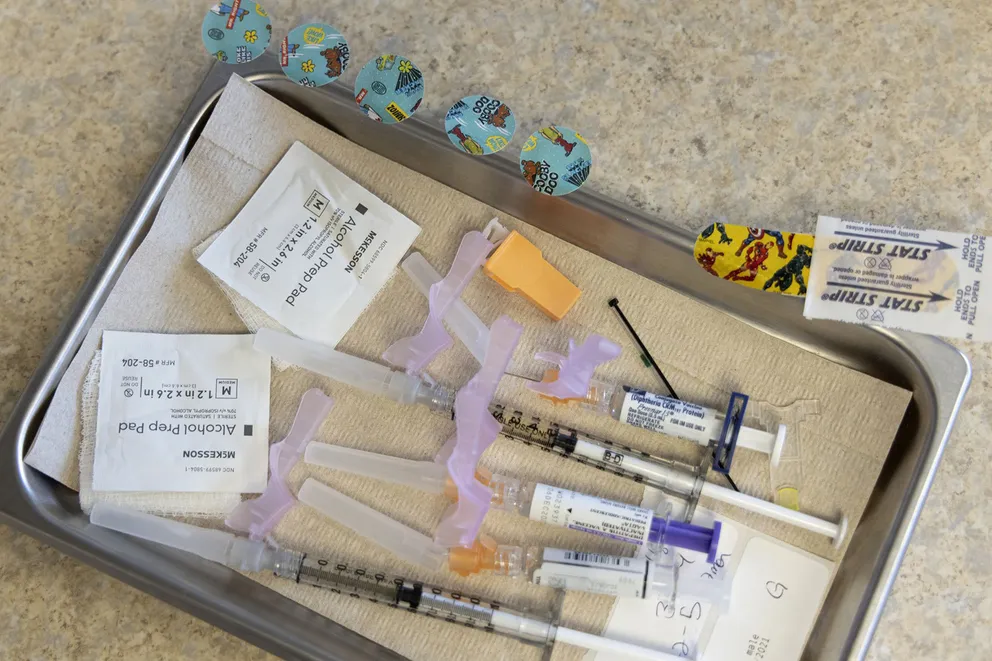
Various vaccines at a children’s hospital in the U.S. on October 18, 2022 | Source: Getty Images
Dr. Amy Thompson, CEO of Covenant Health Lubbock Service Area, confirmed the heartbreaking news during a press conference, stating, “The patient has passed away from complications caused by the measles virus. The child was school-aged and did not reside in Lubbock County.”
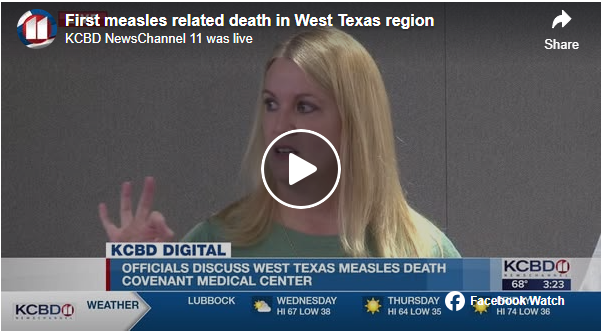
Dr. Thompson extended her condolences, stating, “We do want to say our thoughts and prayers are with this family, as this is new news today, so this is still really fresh for them.”
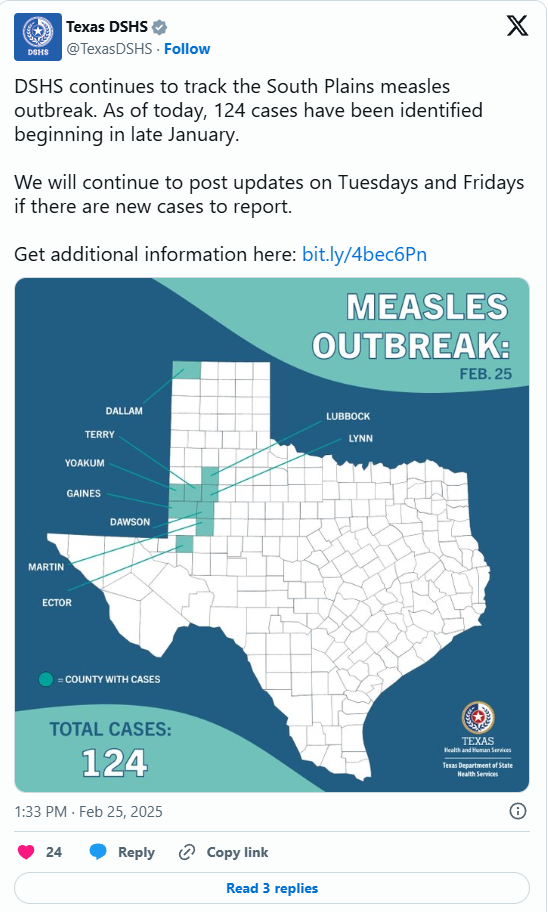
Health officials report that measles cases have surged to 124 since late January, with the majority of infections affecting children. Eighteen individuals have been hospitalized as a result. The Texas DSHS emphasizes that measles is highly contagious and can lead to severe complications, urging the public to take necessary precautions.

The Texas DSHS reports that approximately one in five measles patients require hospitalization, while one in 20 develops pneumonia. In rare cases, the virus can lead to brain swelling and even death. Additionally, measles poses serious risks for pregnant women, potentially causing complications such as premature birth and low birth weight.
Beyond the reported fatality in Lubbock, the Texas DSHS has confirmed measles cases across eight counties. Gaines County remains the hardest hit, reporting 80 cases, followed by Terry County with 21. Dawson County has recorded seven cases, while Yoakum has five, Dallam has four, Martin has three, Ector has two, and Lynn has one. Health officials continue to monitor the outbreak as concerns rise over its rapid spread.
Dr. Lara Johnson, chief medical officer of Covenant Health Lubbock Service Area, addressed concerns about hospital care in a recent CNN interview, clarifying, “We don’t hospitalize patients for quarantine purposes. Quarantine is not something that would happen in a healthcare facility. We admit patients who need acute supportive treatment in our hospital.”
She further explained that some measles patients have required supplemental oxygen and respiratory support due to complications from viral pneumonia associated with the virus.
The Centers for Disease Control and Prevention (CDC) warns that measles is highly contagious and can result in severe complications, especially for babies, young children, pregnant women, and individuals with weakened immune systems. Health officials urge vaccination and preventive measures to curb the outbreak.
Measles symptoms typically emerge 7 to 14 days after exposure, starting with a high fever, cough, runny nose, and red, watery eyes. Within two to three days, tiny white spots known as Koplik spots may appear inside the mouth. By days three to five, a distinctive red rash develops, beginning at the hairline and gradually spreading downward across the body.
Measles can lead to several complications, with ear infections affecting about 1 in 10 children and diarrhea occurring in fewer than 1 in 10 cases. More severe complications include pneumonia and, in rare cases, brain swelling, which can be fatal.
Beyond immediate health risks, measles can also have devastating long-term effects. Subacute sclerosing panencephalitis (SSPE), a rare but fatal disease of the central nervous system, can develop 7 to 10 years after infection, even in individuals who initially appeared to recover. The risk is highest for those who contracted measles before the age of 2.
As cases continue to rise, health officials are stressing the critical importance of vaccination and early recognition of symptoms to prevent further spread of the disease and avoid complications. Public awareness and proactive measures are essential in combating this outbreak and protecting vulnerable populations.
The reported measles-related death in Texas follows closely on the heels of the U.S. confirming its first H5N1 bird flu fatality in January, adding to the serious public health concerns.
The fatal case involved a Louisiana patient, identified as the first severe human case of highly pathogenic avian influenza (HPAI) in the country. This individual, over 65 years old and with underlying medical conditions, tragically passed away, as confirmed by the Louisiana Department of Health (LDH).

Following exposure to both wild birds and non-commercial backyard flocks, the late patient contracted H5N1, resulting in hospitalization. In light of the report on the death, the Louisiana Department of Health (LDH) issued a heartfelt message to the loved ones of the deceased, emphasizing the seriousness of this public health threat and the importance of taking precautions to prevent further cases.

USGS Biologist Science Tech Brooke Hill releases a Western Sandpiper after testing it for the highly pathogenic H5N1 avian influenza in Sonoma, California on August 16, 2006 | Source: Getty Images
“The Department expresses its deepest condolences to the patient’s family and friends as they mourn the loss of their loved one,” they stated. They also clarified that no further updates or details would be provided regarding the deceased patient, respecting the family’s privacy during this difficult time.

In an effort to protect the public, the Louisiana Department of Health (LDH) shared several measures individuals can take to prevent H5N1 infection. They strongly advised people to avoid exposure by steering clear of wild birds and any animals that may be infected with or suspected of carrying bird flu viruses. These precautions are essential in minimizing the risk of transmission and ensuring community safety.

New England Wildlife Center staff rescuing birds affected by an oil spill in Brookline, Massachusetts on December 9, 2024 | Source: Getty Images
Individuals are advised not to bring sick wild animals into their homes and to avoid any contact with them, their droppings, or dead animals. The LDH also warns the public to keep their pets away from wild and deceased animals to reduce the risk of exposure.
As an additional precaution, the LDH recommends against consuming undercooked or raw food. Eggs, poultry, and other animal products should be cooked to the appropriate temperature, and individuals should take care to prevent cross-contamination between raw and cooked foods to ensure safety.
Officials encourage individuals to report any sick or dead birds or animals to the Louisiana Department of Agriculture and Forestry Diagnostic Lab at 318-927-3441 or the USDA at 1-866-536-7593. Additionally, they advise those working on dairy or poultry farms to consult their medical provider about receiving a seasonal flu vaccination to further protect themselves against potential infections. These measures are crucial for safeguarding public health and preventing the spread of diseases.
While receiving the seasonal flu vaccination will not make individuals immune to avian influenza viruses, it may help reduce the risk of co-infection with both flu and avian viruses. The LDH emphasized that although the risk of infection remains low for the general public, individuals who work closely with birds, cows, or poultry, or have recreational exposure to them, face a higher risk of infection. Therefore, taking precautions and staying informed is essential for those in these situations.
The LDH also stated, “If you have been exposed to sick or dead birds or other animals, or work on a farm where avian influenza has been detected, watch for respiratory symptoms or conjunctivitis.”
Individuals who develop symptoms within ten days of exposure to potential sources of the virus should inform their healthcare provider about their contact with sick animals and their concerns regarding avian influenza. Prompt communication with healthcare professionals is vital for early detection and treatment.
Taking these steps helps medical professionals offer appropriate guidance on treatment and testing. The LDH further advised, “Stay home and away from others while you have symptoms.”
In addition to outlining preventive measures and the concerning news about the U.S.’s first H5N1 death, the LDH confirmed that there is no evidence of person-to-person transmission or any additional cases beyond those already reported, following an extensive public health investigation. This information is reassuring as officials continue to monitor the situation closely.
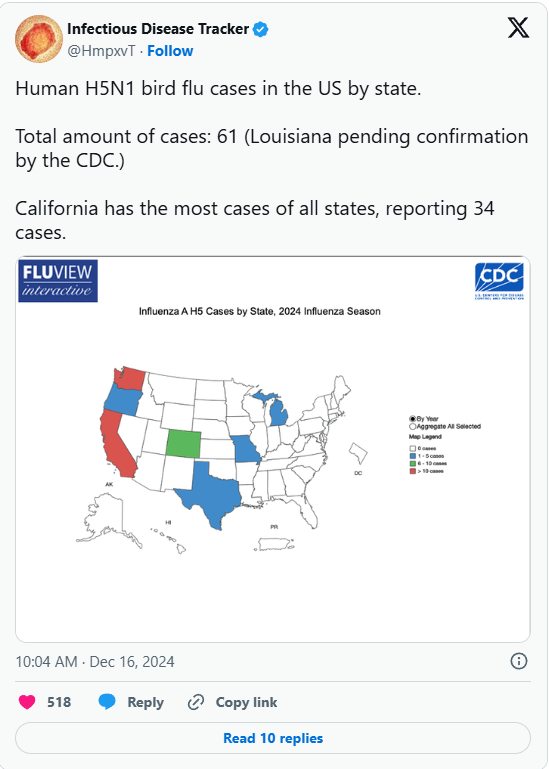
Regarding the current situation, the CDC reported a confirmed total of 66 human cases in the U.S. during the 2024 outbreak, with several recent cases primarily affecting dairy and poultry workers.
These human cases have been reported across multiple states, including California, Colorado, Iowa, Louisiana, Michigan, Missouri, Oregon, Texas, Washington, and Wisconsin. Health officials continue to monitor the outbreak closely to ensure public safety and implement necessary measures.
Regarding exposure sources, 36 of the 37 cases in California were linked to dairy herds (cattle), while one case remains with an unknown source. In Colorado, there were ten reported cases, with one stemming from dairy herds (cattle) and the remaining nine originating from poultry farms and culling operations. This data highlights the importance of monitoring and controlling potential sources of infection in agricultural settings.

A cattle ranch in Panama in 2024. | Source: Getty Images
In Iowa, the single reported case was traced back to poultry farms and culling operations, while the case in Louisiana, which resulted in the patient’s death, was linked to exposure to other animals.
Michigan reported two cases, both stemming from dairy herds (cattle), and the case in Missouri had an unknown exposure source. Additionally, Oregon and Wisconsin each recorded one case connected to poultry farms and culling operations. This information underscores the significance of vigilance in monitoring potential exposure sources in the agricultural sector.

The exposure source for the Texas case was linked to dairy herds (cattle), while all 11 cases in Washington originated from poultry farms and culling operations. Additionally, the CDC reported that as of January 3, 2025, H5N1 bird flu had been detected in 10,922 wild birds.
Before sharing the current data—emphasizing that it is subject to continuous updates as the situation evolves—officials had been investigating the source of the Louisiana patient’s H5N1 bird flu infection, highlighting the ongoing efforts to understand and control the outbreak.
Before the exposure source was confirmed, it was initially believed that the Louisiana patient had come into contact with deceased birds from backyard flocks. This marked the first reported U.S. case of H5N1 bird flu linked to backyard flock exposure, raising additional concerns about the virus’s spread in non-commercial settings.

Genomic analysis of the H5N1 bird flu virus from the Louisiana patient revealed that it belongs to the D1.1 genotype, which has been linked to recent detections in wild birds and poultry in the U.S., as well as human cases in Canada and Washington.
This genotype differs from the B3.13 genotype, which has been associated with dairy cows, some human cases, and poultry outbreaks. At the time, the CDC was conducting further genomic sequencing and virus isolation from the sick patient to better understand the virus’s spread and potential variations.

A single severe H5N1 bird flu case in a person is not unusual, as the virus has caused serious illness and fatalities in other countries. Despite this, the CDC has maintained that the overall public health risk from H5N1 bird flu remains low.
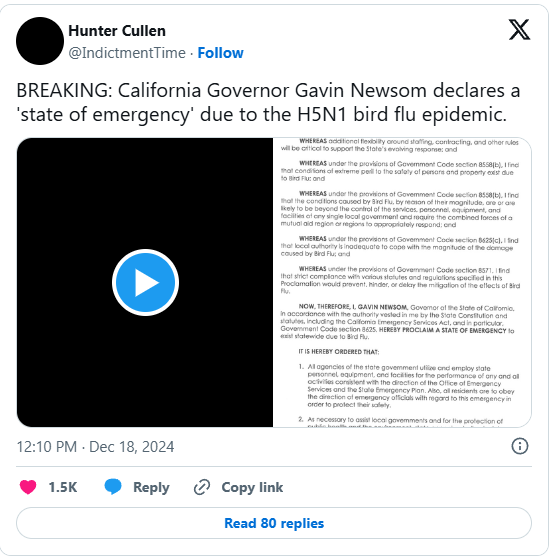
However, in response to the outbreak, California Governor Gavin Newsom declared a State of Emergency to accelerate the state’s efforts in managing the spread of H5N1 bird flu after cases were detected in Southern California dairy cows. This move aims to enhance containment measures and protect both public health and the agricultural industry.
The H5N1 bird flu virus has spread across 16 states since its first confirmed detection in Texas and Kansas on March 25, 2024. The virus was initially identified in the U.S. wild bird population in South Carolina in January 2022, followed by California in July 2022.
An outbreak in dairy cows was reported in Texas and Kansas, prompting the California Department of Food and Agriculture (CDFA) to monitor herds in California. As of December 2024, 61 confirmed human cases had been reported across seven states, with 34 of those cases in California, highlighting the ongoing spread and impact of the virus.
Governor Newsom explained that the State of Emergency declaration allows for greater flexibility in staffing, contracts, and containment measures, ensuring a swift and effective response. He reassured the public that California has implemented the most extensive testing and monitoring system in the nation to combat the outbreak, emphasizing the state’s commitment to controlling the spread of H5N1 bird flu and protecting both public health and agriculture.
Governor Newsom stated, “We are committed to further protecting public health, supporting our agriculture industry, and ensuring that Californians have access to accurate, up-to-date information.” His remarks underscore the state’s proactive approach in managing the outbreak and reinforcing public confidence in containment efforts.
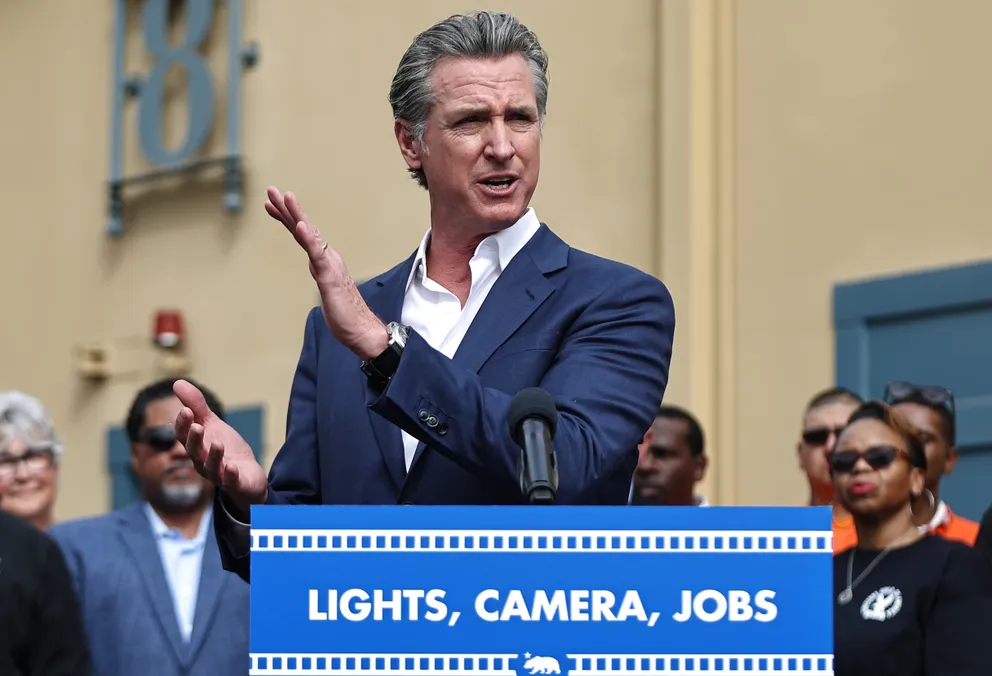
California Governor Gavin Newsom speaks during a press conference in Los Angeles, California, on October 27, 2024 | Source: Getty Images
As the government works to strengthen public health measures, individuals are urged to reduce their risk of H5N1 exposure whenever possible. In situations where exposure is unavoidable, personal protective equipment (PPE) should be used, including gloves, safety goggles, N95 respirators, and disposable coveralls, to minimize the risk of infection. These precautions are essential for anyone who may be in close contact with potentially infected animals or environments.
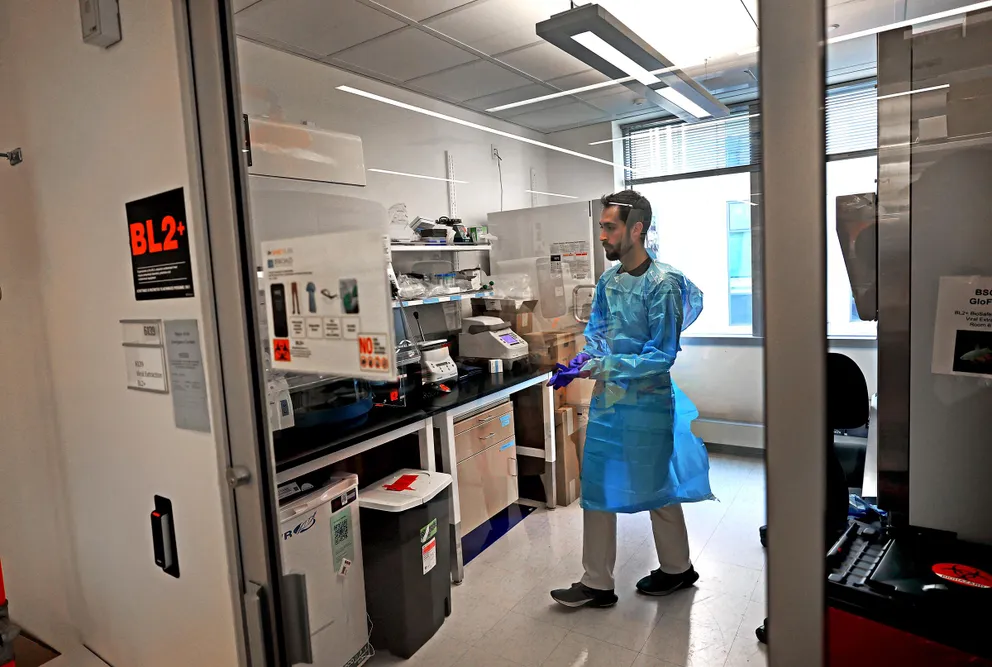
Jon Arizti Sanz, PhD, Postdoctoral Fellow testing purchased milk at area grocery stores for the presence of bird flu, in Cambridge on May 14, 2024 | Source: Getty Images
For poultry and livestock workers, employers are urged to update workplace health and safety plans to address potential H5N1 exposure. Conducting thorough hazard assessments to identify high-risk tasks is also recommended to enhance workplace safety.
Additionally, by implementing control measures such as isolating infected animals, enforcing strict hygiene protocols, and providing appropriate protective equipment, employers can significantly reduce the risk of transmission and safeguard both workers and livestock.

Ducks with bird flu also known as poultry flu are collected and put in a container in Zarnewanz, Germany on November 28, 2024 | Source: Getty Images
Employers should ensure that workers are provided with appropriate personal protective equipment (PPE) to minimize the risk of contact with infected animals or contaminated materials. Proper training on PPE use, hygiene practices, and biosecurity measures is also essential.
By implementing these precautions and adhering to recommended safety protocols, the spread of H5N1 can be effectively controlled, protecting both workers and the broader community.